By Joshua Beltran, Research Assistant, Center for Health Equity Engagement Education and Research
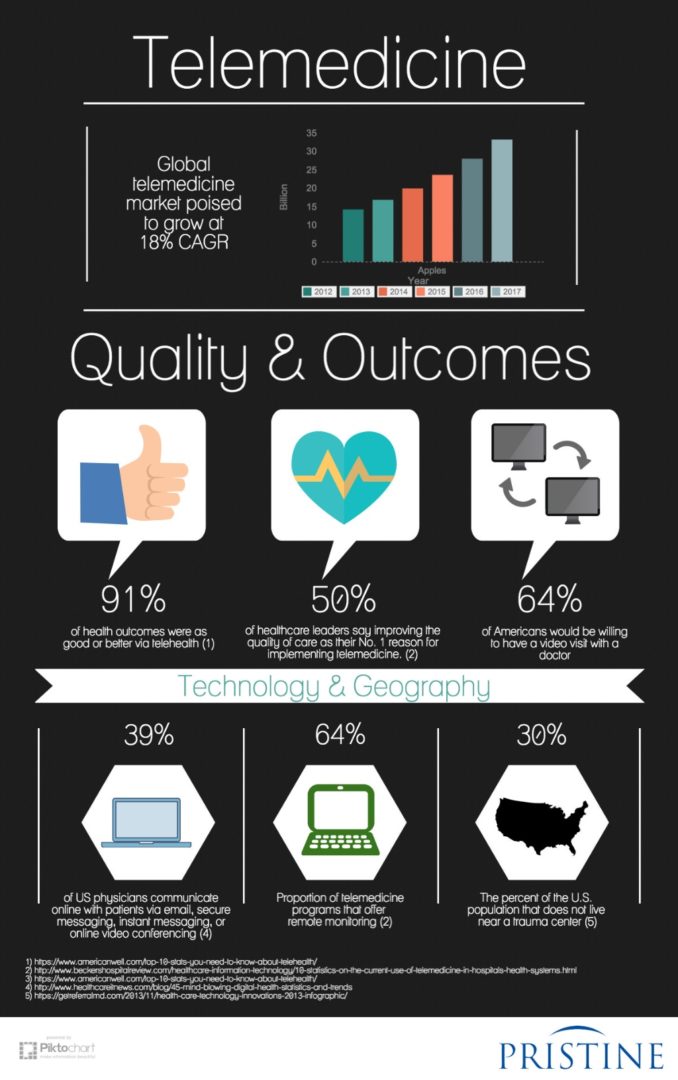
One significant thing the pandemic has proven is that the ability to transition to remote work without losing quality or efficiency is more common and achievable than initially thought. One area that may surprise some is medical care in the form of telehealth/telemedicine. Now, telehealth in and of itself is not entirely new, but the pandemic really pushed it to the forefront and highlighted its ability to provide quality health care without in-person visits. Additionally, the pandemic forced telehealth to evolve by improving the quality of care, expanding the services available, as well as increasing ease of access and use. Although the delta variant is halting the full return to normalcy, the end of the pandemic is easier to see than it was this time last year. Depending on where you live many of the restrictions have been lifted, especially for those who have been vaccinated. With the end somewhat in sight, it becomes necessary to re-evaluate the benefits and necessity of remote work like telehealth, and to see if the transitions have a permanent place moving forward. In this article Albert Ferreira, director of telehealth operations at MetroHealth, says that “telehealth is likely here to stay.” This sentiment is backed up in the article by Chris Verdi who is the president of Parafill, “a pharmacy that operates on a mobile and distance platform.” Parafill, fulfills orders by getting prescriptions directly from doctors’ offices and then delivering them to people’s houses. As I said, services like Parafill are finding ways to adapt and expand by increasing their usefulness and services. According Verdi they are looking to include mobile health visits and aim to process prescriptions themselves. He mentions the new aspect of “remote patient monitoring”, which will allow doctors to check things like blood sugar and blood pressure via wearable technology. I previously mentioned increasing ease of access which is something that Mr. Verdi is also privy to by stating “As the baby boomer generation continues to become pretty tech comfortable, a lot can be done by doctors and their offices in monitoring patient conditions based on the use of wearables to monitor people’s health.” These benefits and more can be seen as long as telehealth services continue stay operational as well as evolve.
 However, telehealth is not free from the constraints and regulations of the American medical system and United States’ government policies. An article from STAT news, “The party is winding down”: States and insurers resurrect barriers to telehealth, putting strain on patients”, illustrates the biggest issues telehealth is facing in just its title. It seems that provisions that were put in place by States and insurance companies at the start of the pandemic, as a way to encourage patients to engage with telehealth services, are in the process of being phased out. Conversely, the prior regulations that contribute to making telehealth convoluted and costly are being reinstated. I see this as a major step in the wrong direction for a few reasons. First, the pandemic is not over and although restrictions in many places have been lifted, the delta variant is leading toward a resurgence. By resurrecting pre-pandemic barriers this causes patients to either forgo treatments and visits or forces them into in-person visits increasing possible exposure. Either way, patient care is being impacted severely. Second, telehealth visits increase convenience for both patients and doctors because simple screenings or checks can have their time alleviated by telehealth. A way telehealth does this is by eliminating a patient’s time to travel to the doctor’s office and diminishing the necessity of time slots thereby freeing up time for doctors. Also, telehealth isn’t just economically sound for patients but for doctors as well. The highlights a primary physician who has been able to treat patients across different states. This was viable because emergency orders from the state governors and licensing boards, expedited the application process or extended telehealth licenses to providers in neighboring states. Normally, a license in each state would had to have been obtained, a process which can take possibly months to finalize and cost hundreds of dollars to the physician. Lastly, these restrictions impact continuity of care, not just regarding the pandemic, but specifically with doctor-patient relationships. The article points to patients who were apprehensive toward therapy may not be inclined to continue their sessions with a new therapist that they do not know. Finding the right therapist is already a challenging task, but telehealth was a way to aid the search.
However, telehealth is not free from the constraints and regulations of the American medical system and United States’ government policies. An article from STAT news, “The party is winding down”: States and insurers resurrect barriers to telehealth, putting strain on patients”, illustrates the biggest issues telehealth is facing in just its title. It seems that provisions that were put in place by States and insurance companies at the start of the pandemic, as a way to encourage patients to engage with telehealth services, are in the process of being phased out. Conversely, the prior regulations that contribute to making telehealth convoluted and costly are being reinstated. I see this as a major step in the wrong direction for a few reasons. First, the pandemic is not over and although restrictions in many places have been lifted, the delta variant is leading toward a resurgence. By resurrecting pre-pandemic barriers this causes patients to either forgo treatments and visits or forces them into in-person visits increasing possible exposure. Either way, patient care is being impacted severely. Second, telehealth visits increase convenience for both patients and doctors because simple screenings or checks can have their time alleviated by telehealth. A way telehealth does this is by eliminating a patient’s time to travel to the doctor’s office and diminishing the necessity of time slots thereby freeing up time for doctors. Also, telehealth isn’t just economically sound for patients but for doctors as well. The highlights a primary physician who has been able to treat patients across different states. This was viable because emergency orders from the state governors and licensing boards, expedited the application process or extended telehealth licenses to providers in neighboring states. Normally, a license in each state would had to have been obtained, a process which can take possibly months to finalize and cost hundreds of dollars to the physician. Lastly, these restrictions impact continuity of care, not just regarding the pandemic, but specifically with doctor-patient relationships. The article points to patients who were apprehensive toward therapy may not be inclined to continue their sessions with a new therapist that they do not know. Finding the right therapist is already a challenging task, but telehealth was a way to aid the search.
This past year has proven not only that remote work, like telehealth, can work but also that in some cases it is the more efficient and suitable option. By all measures these barriers start to negate the progress that has been made. I feel that bringing back pre-pandemic parameters not only hinders telehealth’s execution and usefulness but impedes its ability to evolve, expand, and improve.